AIMS:
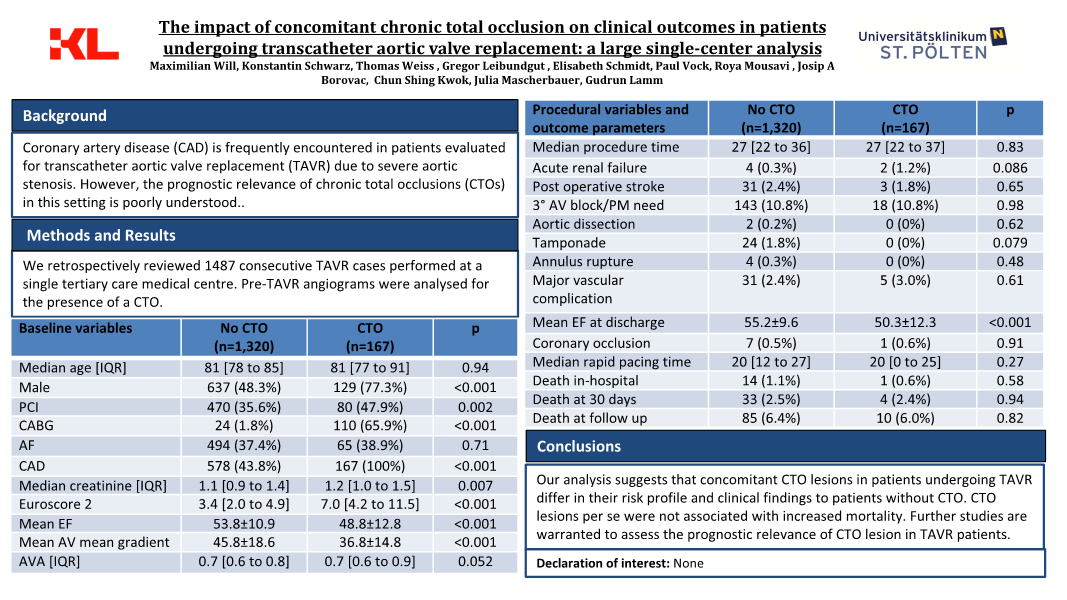
Coronary artery disease (CAD) is frequently encountered in patients evaluated for transcatheter aortic valve implantation (TAVI) due to severe aortic stenosis. However, the prognostic relevance of chronic total occlusions (CTOs) in this setting is poorly understood. We aimed to assess the impact of CTOs on clinical outcomes in patients undergoing TAVI in a large single center cohort.
METHODS AND RESULTS:
We retrospectively reviewed 1487 consecutive TAVI cases performed at a single tertiary care medical center. Pre-TAVI angiograms were analyzed for the presence of a CTO. At the time of TAVI, 11.2% (n = 167) patients had a CTO. Relevant comorbidities were more prevalent in the CTO cohort (hypertension (85.6% vs. 78.8%) (p = 0.039), dyslipidemia 88.0% 65.8% (p < 0.001)) diabetes mellitus 40.1% vs. 32.7% (p = 0.057). Median creatinine levels were slightly higher in the CTO group in our cohort (1.2 mg/dL, IQR: 1.0 to 1.5) vs (1.1 mg/dL, IQR: 0.9 to 1.4) (p = 0.007). Naturally, the presence of angina was significantly higher in the CTO group (8.4%) vs. (3.4%) (p = 0.002) and a higher proportion of patients with prior myocardial infarction (10.8%) vs (2.3%) (p < 0.001) was detected. Consistently, PCI and CABG were more frequently performed in the CTO group (47.9%) compared to the no CTO group (35.6%) (p = 0.002) and (65.9%) vs. (1.8%) (p < 0.001), respectively. Notably, the CTO group showed a higher prevalence of left main stem disease compared to the no CTO group (57.5% vs. 4.1%, p < 0.001). Consequently, Euroscore and Euroscore 2 were all significantly higher in the CTO group compared to the no CTO group (p < 0.001 for all). At discharge, patients in the CTO group had a significantly lower mean ejection fraction (50.3% ± 12.3%) compared to the no CTO group (55.2% ± 9.6%) (p < 0.001). The mean aortic valve mean gradient was significantly higher in the no chronic total occlusion (CTO) group (45.8 mmHg ± 18.6) compared to the CTO group (36.8 mmHg ± 14.8) (p < 0.001). In-hospital death, death at 30 days, and death at mean follow-up after 1,9 years, did not show significant differences between the two groups (all p > 0.05). In a subgroup analysis this study compared patients with CTOs undergoing TAVI based on the presence or absence of viability. The results revealed significantly higher 30-day and follow-up mortality rates in the CTO no viability group (p=0.008 and p=0.024, respectively),
CONCLUSION:
Our analysis suggests that concomitant CTO lesions in patients undergoing TAVI with concomitant CTO lesions differ in their risk profile and clinical findings to patients without CTOs. CTO lesion per se were not associated with increased mortality, nevertheless CTOs which supply non-viable myocardium in TAVI population were associated with increased risk of death. Further studies are warranted to assess the prognostic relevance of CTO lesion in TAVI patients.NULLNULL