AIMS:
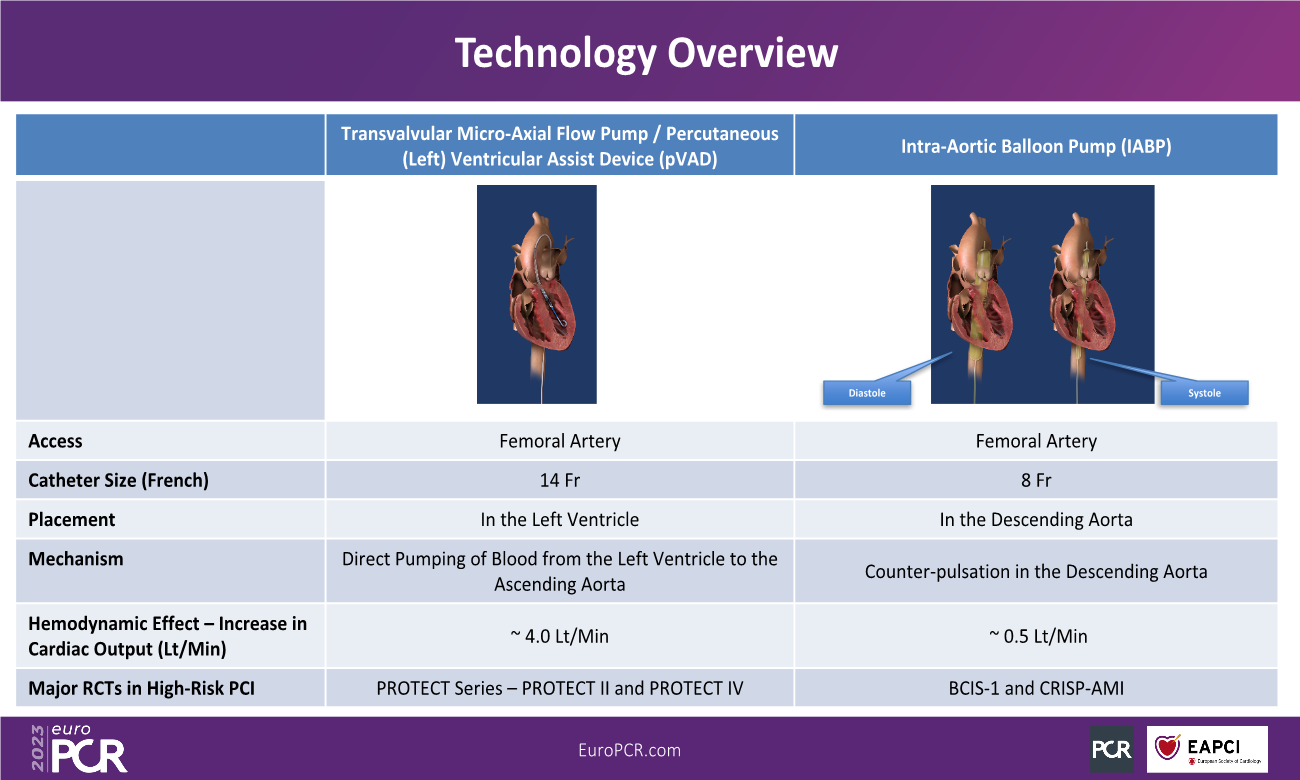
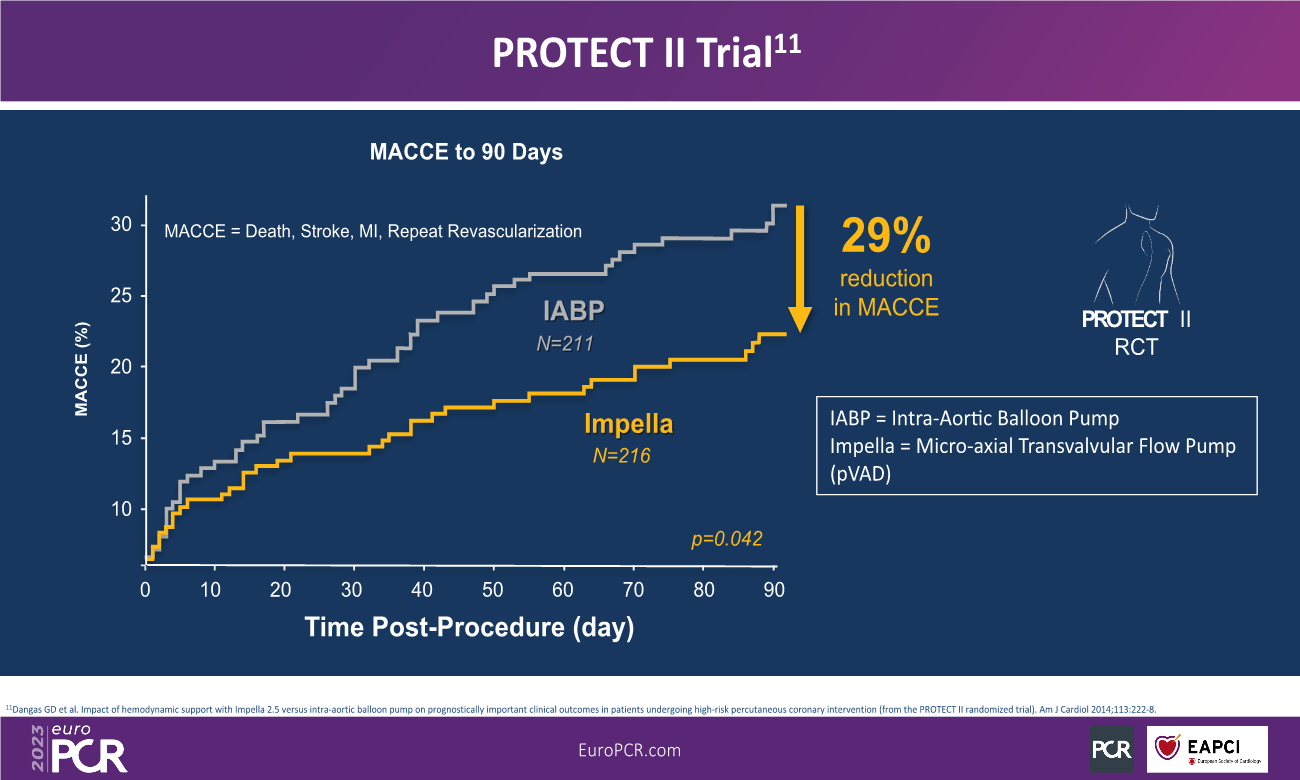
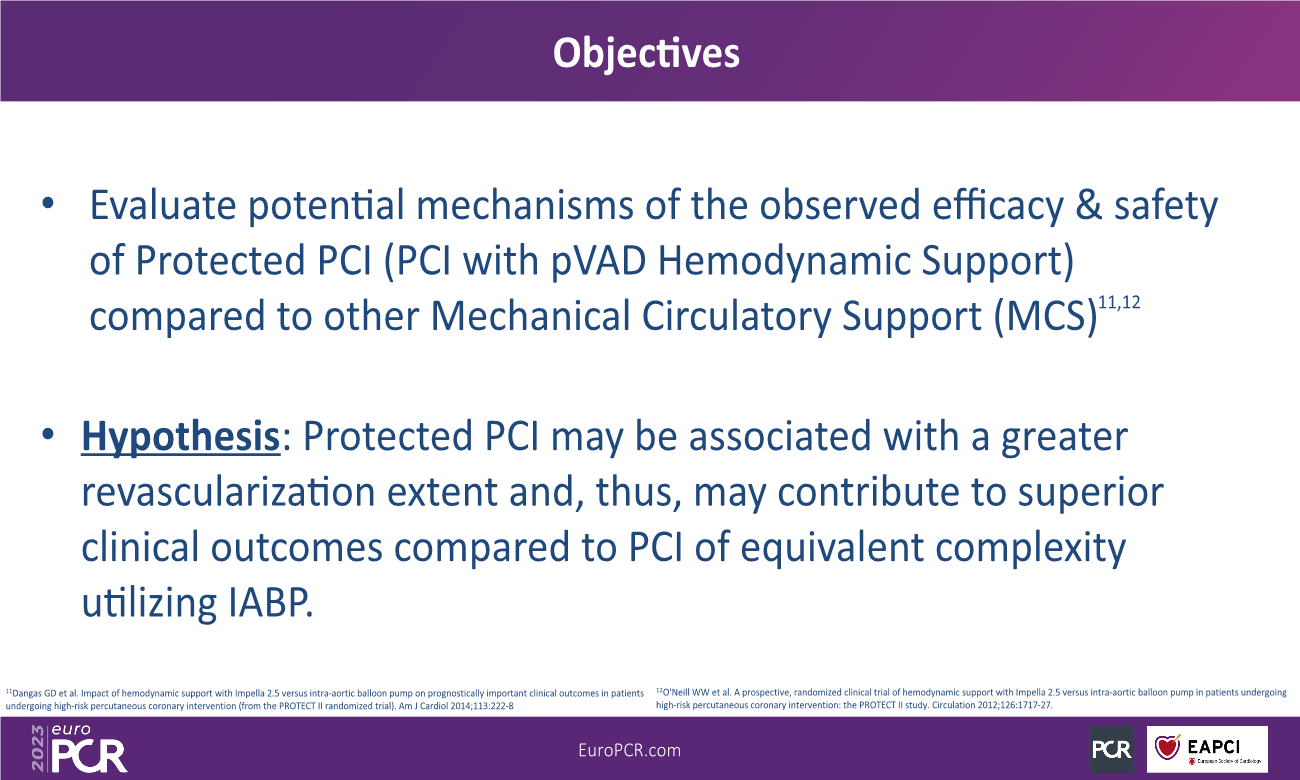
Prior studies have shown that complete revascularisation (CR) during percutaneous coronary intervention (PCI) is associated with improved long-term patient outcomes. Severity of coronary disease pre-PCI is commonly quantified with the SYNTAX Score (SS) and post-PCI with the residual SS (rSS). In High-Risk PCI, trans-axial percutaneous Left Ventricular Assist Devices (pLVADs) provide greater forward flow compared with intra-aortic balloon pumps (IABPs). We thus hypothesized that CR (as measured by rSS<2) could be achieved more commonly with pLVAD.
METHODS AND RESULTS:
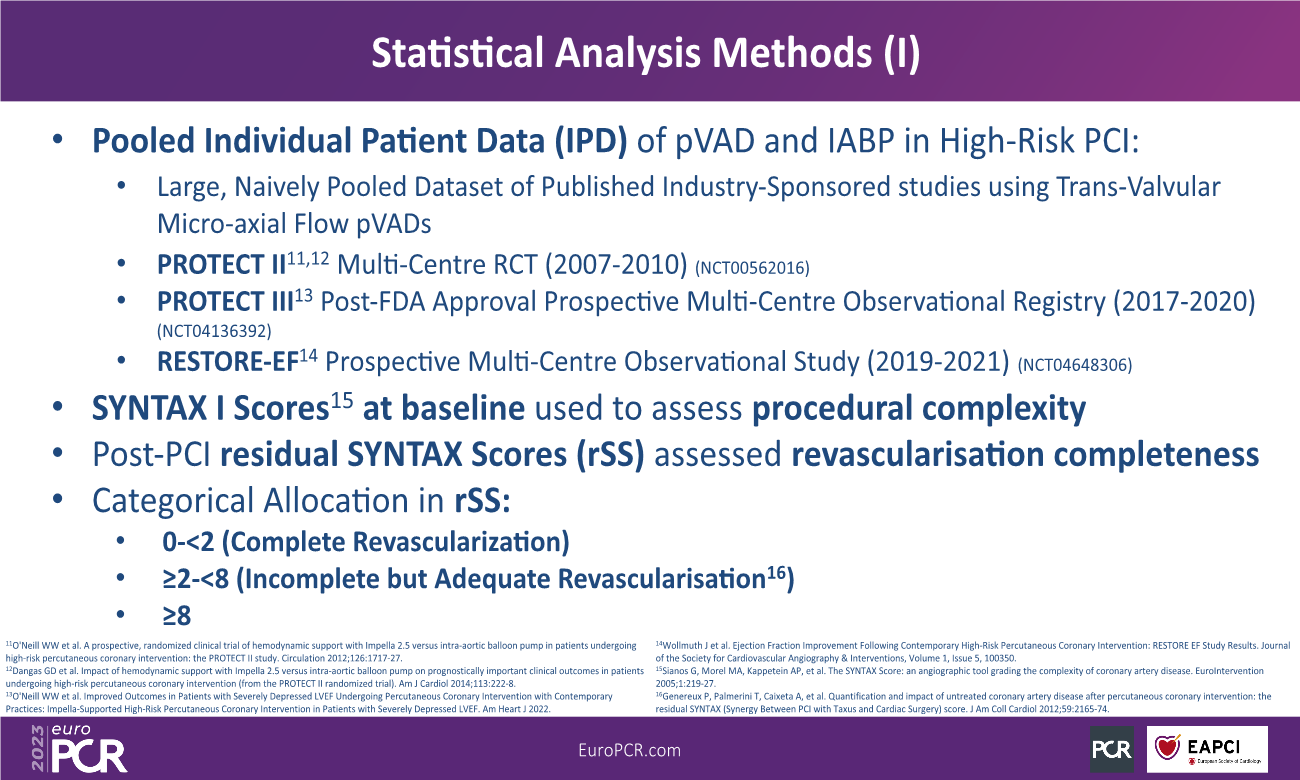
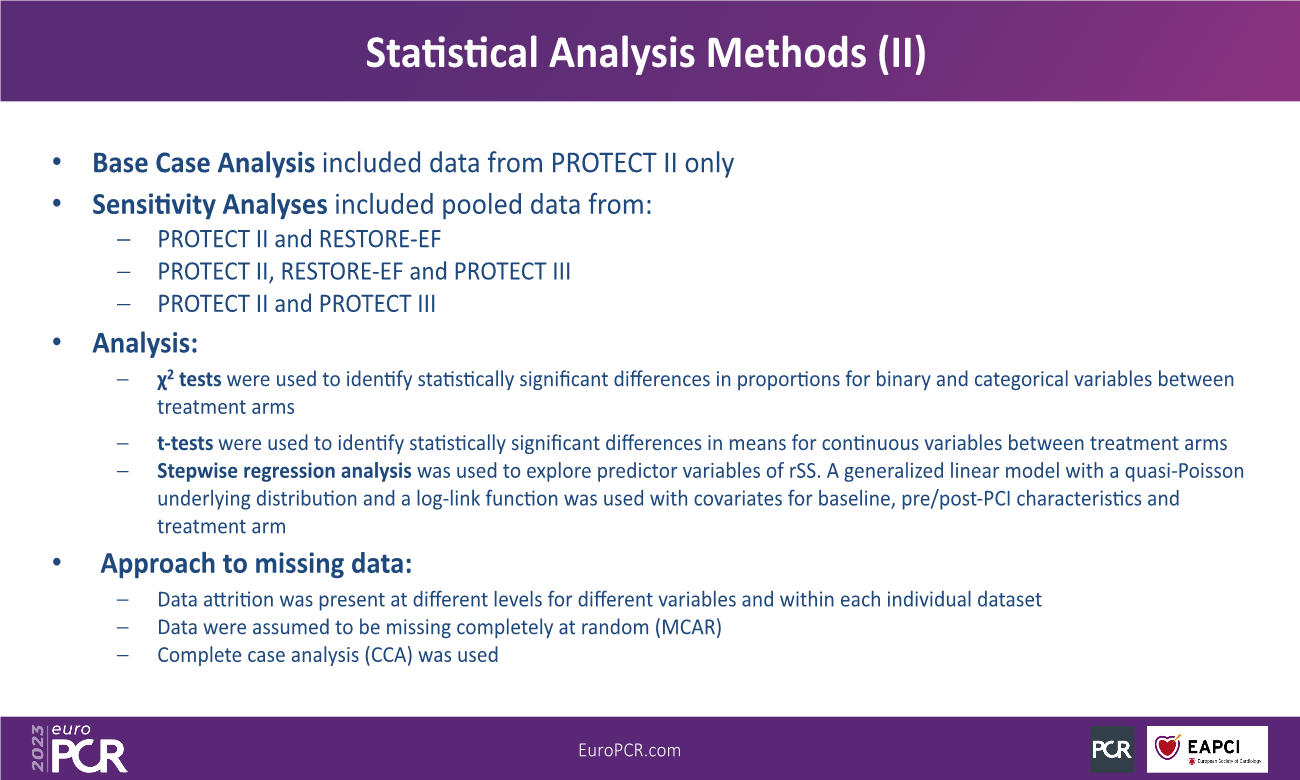
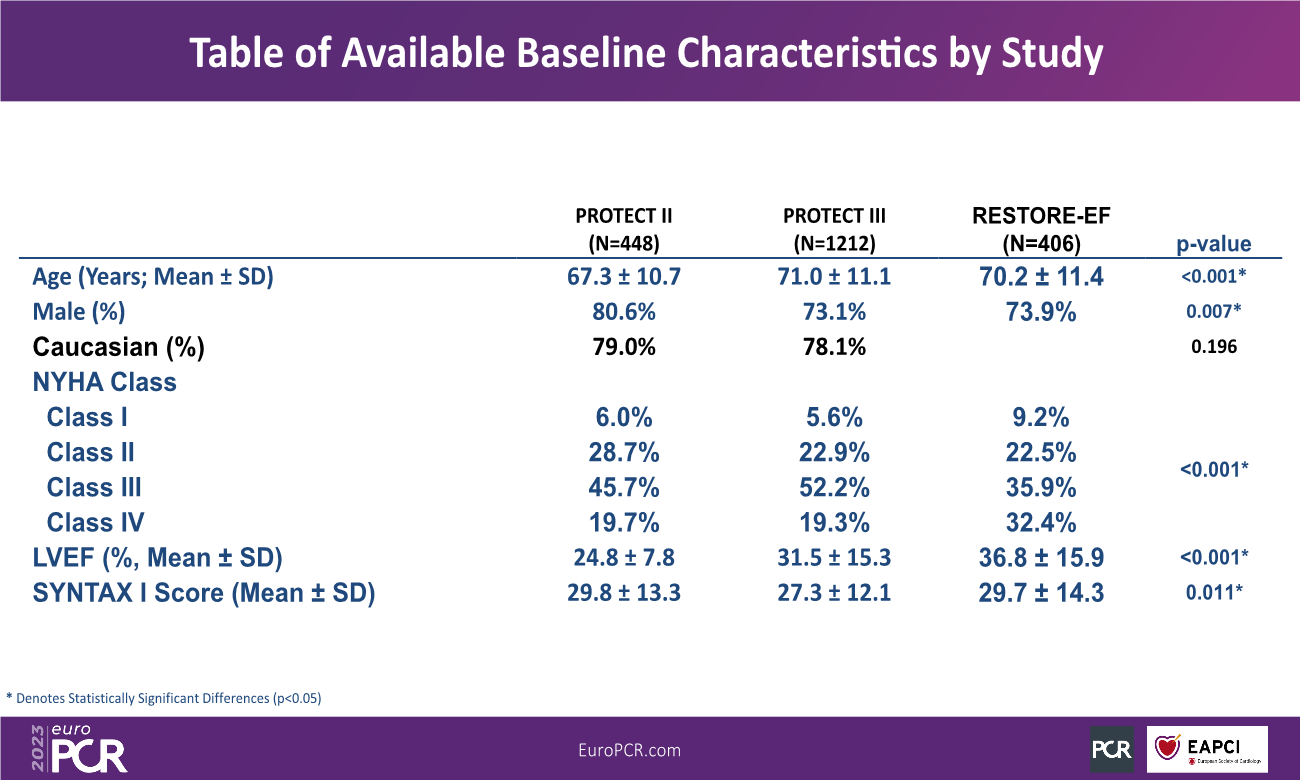
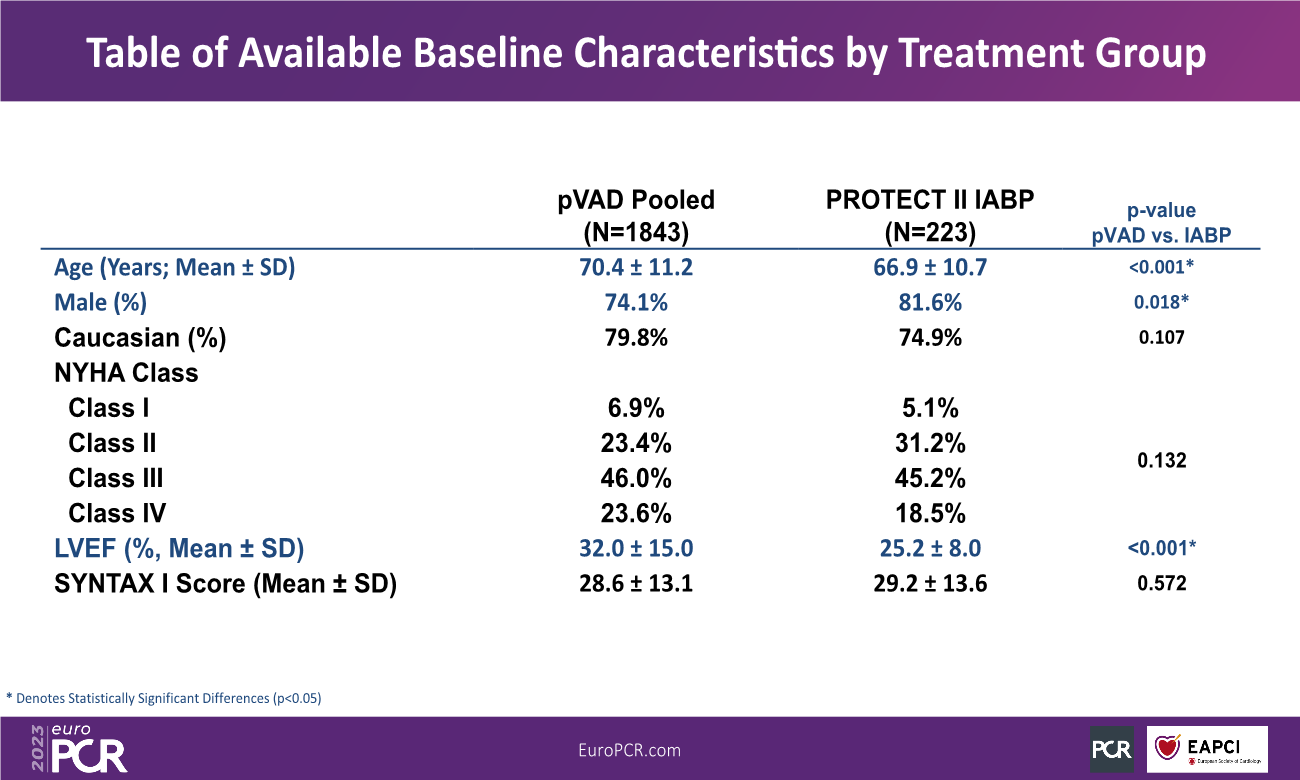
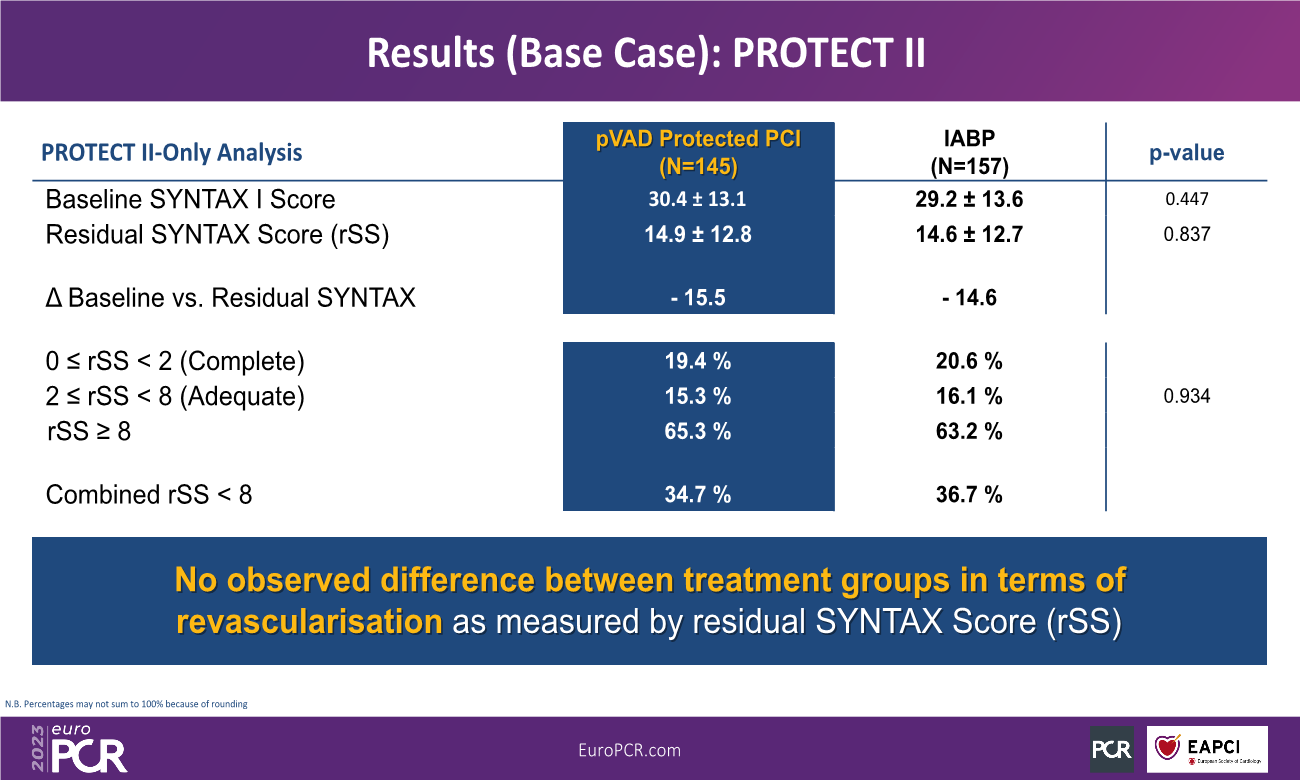
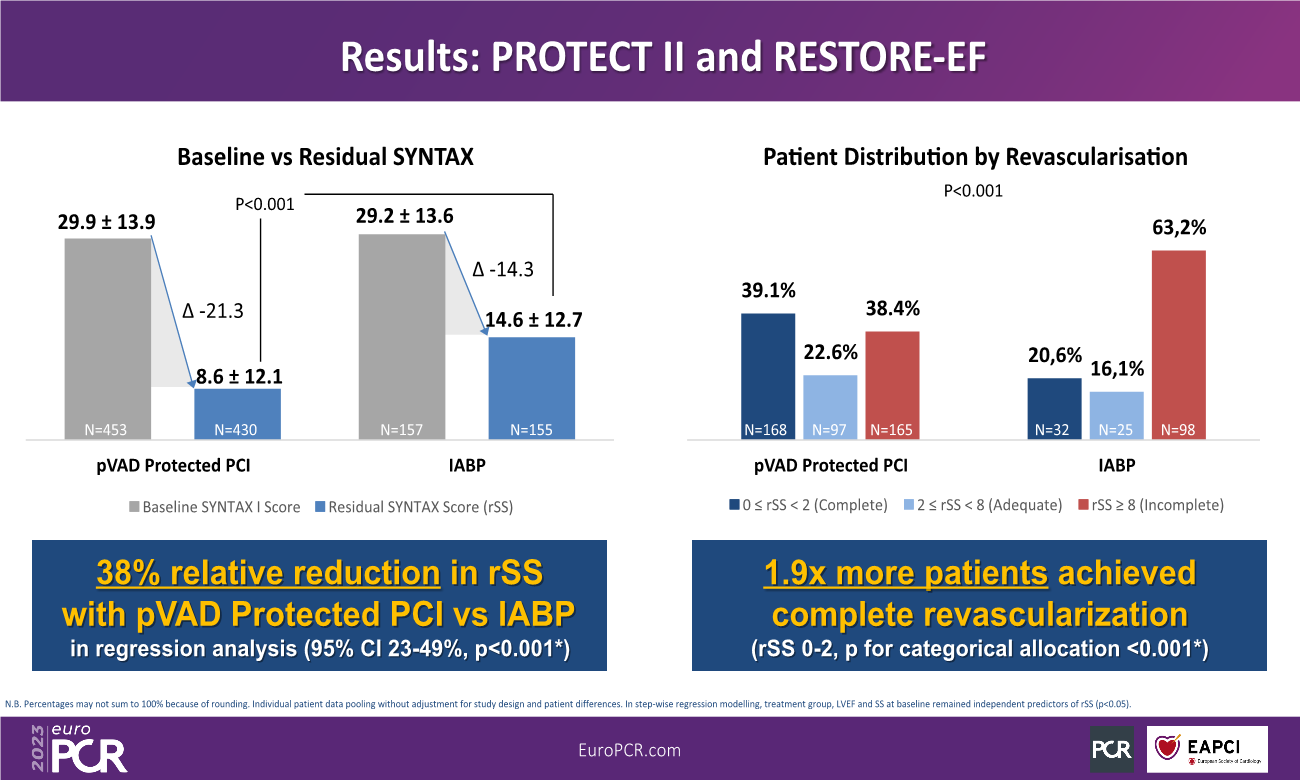
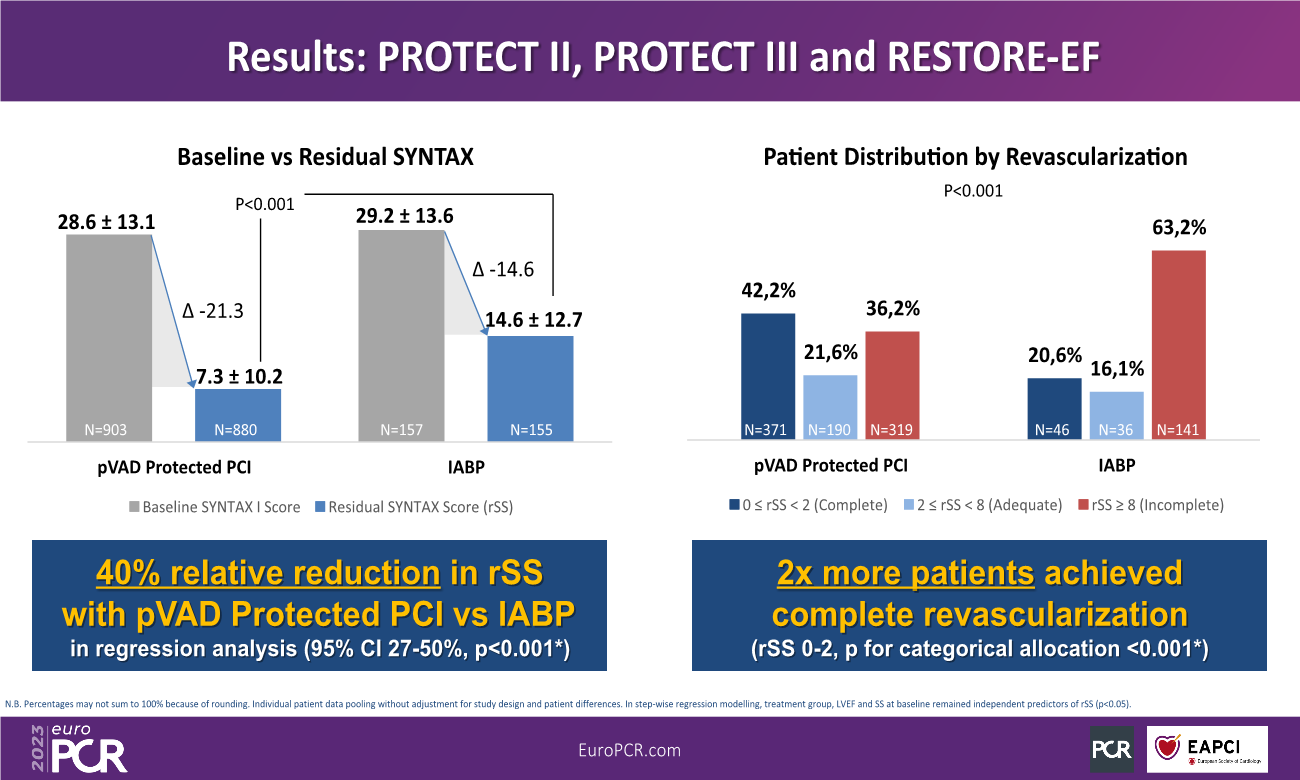
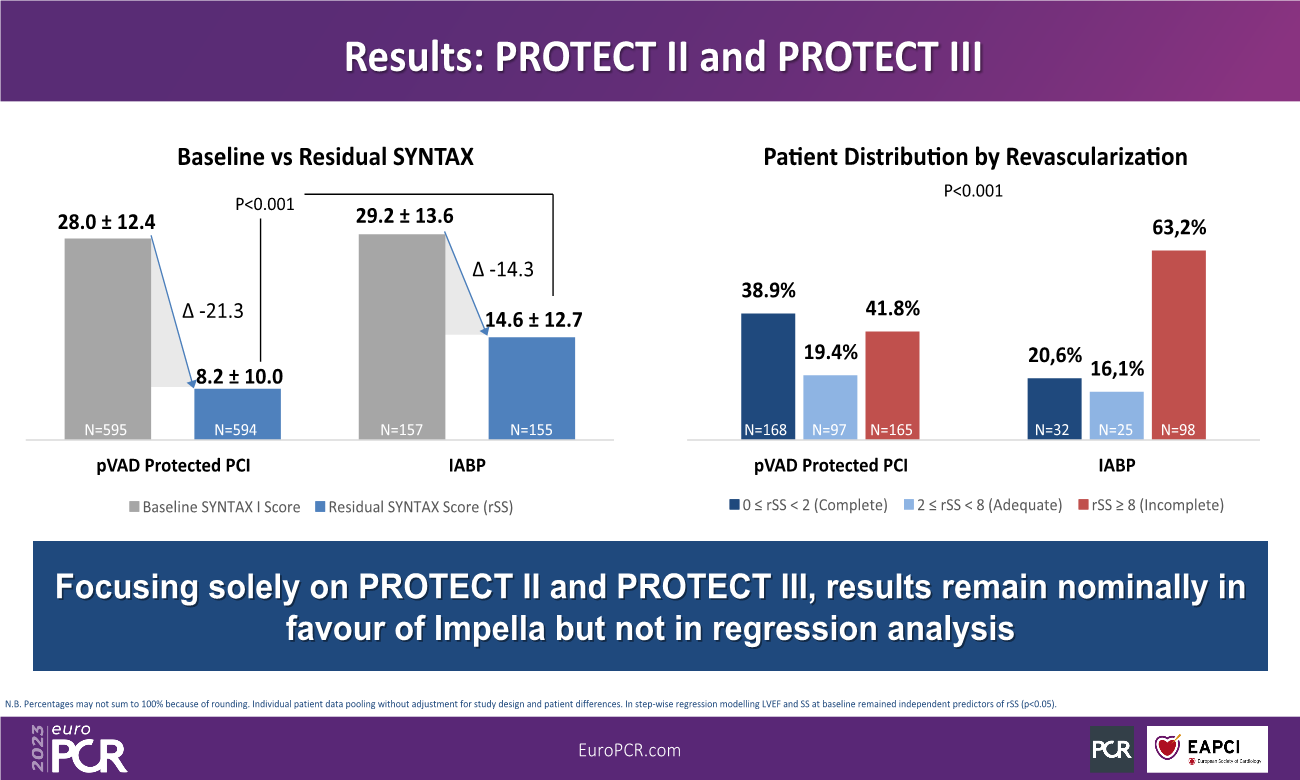
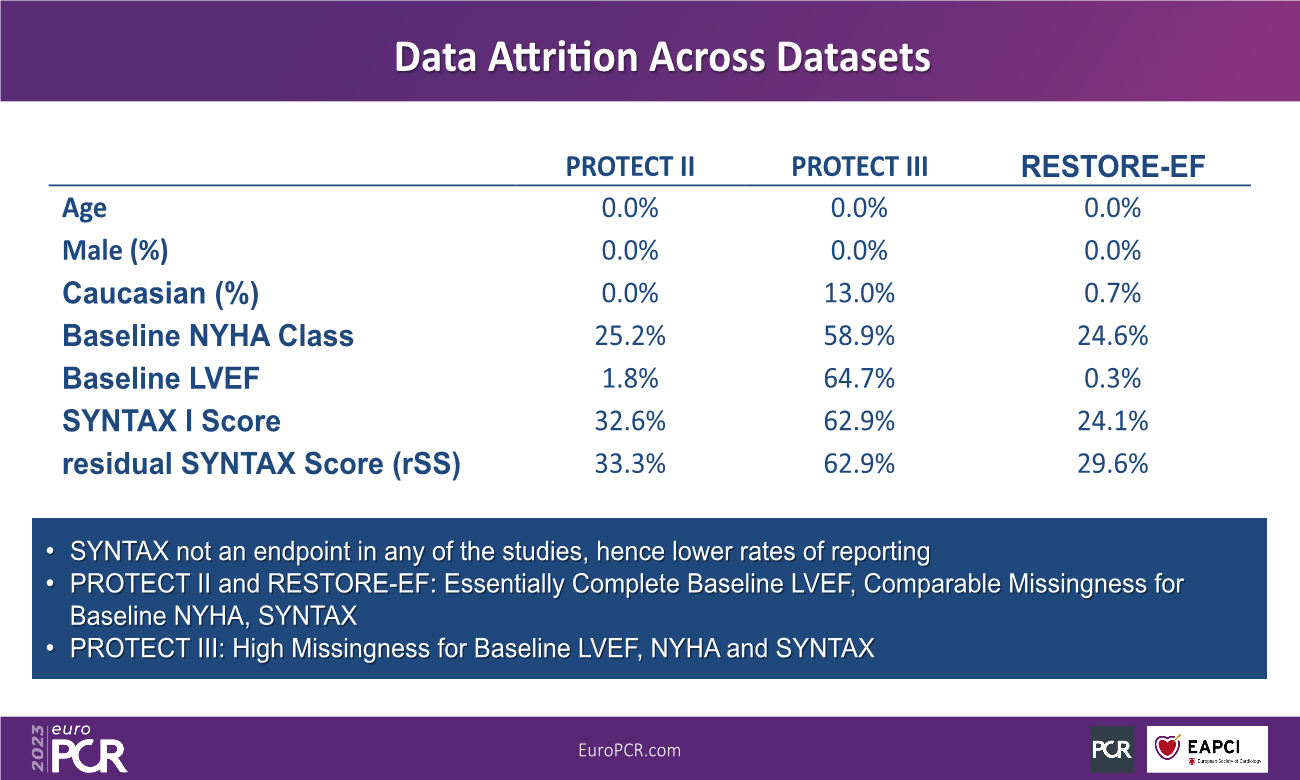
Individual patient data (IPD) from the PROTECT II (NCT00562016), PROTECT III (NCT04136392) and RESTORE-EF (NCT04648306) prospective studies of pLVAD during High-Risk PCI (HR-PCI) were pooled. Regression analyses were performed using generalized linear models with an assumed quasi-Poisson distribution and a log-link for each of the models. All models included covariates adjusted for multiple baseline differences and were refined using stepwise deletion (threshold=0.05). When missingness was above 50% within any dataset, it was excluded from the base-case. Residual SS was compared for pLVAD vs. IABP via mean and categorical allocation (rSS<2, 2-8, ≥8). Angiographic core laboratory analysis of SS and rSS was performed in PROTECT II and III, while RESTORE-EF was site-reported. Sensitivity analyses were performed on core laboratory analyzed data only. 1,733 patients with sufficient information for CR analysis were identified (pLVAD N=1,578; IABP N=155). Baseline SS was similar between pLVAD and IABP (29.9±13.92 vs. 29.2±13.6 respectively, p=0.607). The SS reduction after pLVAD-assisted PCI was 44.3% greater compared with IABP-assisted PCI (21.34±0.13 vs. 14.79±0.41, p<0.001). The post-PCI rSS was lower after pLVAD compared with IABP (8.56±12.13 vs. 14.61±12.7, p<0.001). CR was achieved in 39.1% of pLVAD vs. 20.6% of IABP patients (p<0.001) or 1.9x more patients. In regression analysis, treatment group, among others, remained a statistically significant independent predictor of rSS. IABP patients were overall 58.72% less likely to achieve CR (OR for CR IABP vs. pLVAD 0.4128; 95% CI 0.2762-0.6171; p<0.0001). In the pre-specified subgroup of patients with baseline LVEF ≤20%, baseline SS was again similar for pLVAD and IABP (28.47±14.7 vs. 31.42±14.35 respectively, p=0.18). The SS reduction with pLVAD in this subgroup was 35.1% greater to IABP (19.83±0.34 vs. 14.68±0.72, p<0.001), and post-PCI rSS was lower after pLVAD (8.64±14.34 vs. 16.74±12.71, p=0.0002). CR with pLVAD in this subgroup was achieved more frequently (38.5% pLVAD vs. 15.1% IABP; p=0.001) or in 2.4x more patients. In this subgroup, IABP patients were 71.6% less likely to achieve CR (OR for CR IABP vs. pLVAD 0.2844; 95% CI 0.1285-0.6296; p=0.0019).
CONCLUSION:
This patient-level meta-analysis of angiographic outcomes following pLVAD vs. IABP for patients undergoing HR-PCI shows that CR is achieved significantly more frequently with pLVAD, including in the most critical patients with low EF (≤20%). Since CR is a predictor of improved long-term clinical outcomes, this data may help to inform decisions regarding the type of hemodynamic support for HR-PCI. Thus, we hypothesize that Protected PCI with trans-axial pLVADs might contribute to improved long-term patient outcome by improving the completeness and quality of revascularization, compared to IABP. Ongoing studies are testing this hypothesis.